Misconception #1. Thermography is a non-contact way of taking someone’s temperature.
Fact – It’s not. Core temperature cannot be accurately evaluated by measuring skin temp. There is no conduction of core temperature past the subcutaneous level.
Misconception #2. Measuring skin temperature detects fever.
Fact – Fever will not always produce elevated temperatures at the skin surface.
Misconception #3. Thermography can only detect disease and infection once it is symptomatic.
Fact – Thermal imaging does have the potential to detect developing pathology related to non symptomatic disease before inflammatory symptoms are produced.
Misconception #4. Thermography looks for specific temperatures to detect fever.
Fact – A significant number of symptomatic fevers with elevated core temperature will produce decreased skin temperatures due to perspiration (evaporative cooling).
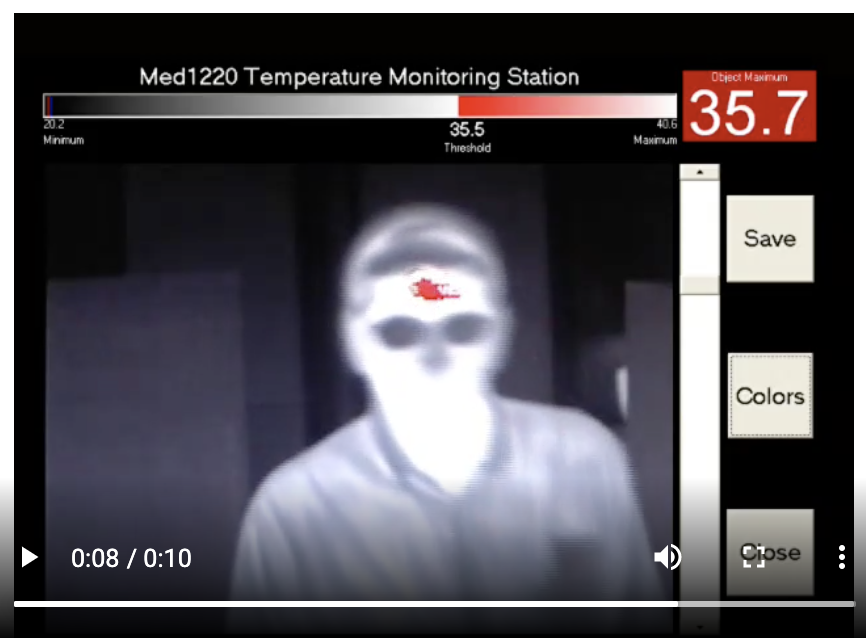
Misconception #5. Use of an external black body reference makes a threshold alarm accurate.
Fact – Radiometric Screening for an absolute temperature threshold, is limited and is dependent on the skill and attention of the technician. The level of false positives produced when setting a manual threshold generally results in technicians setting the threshold higher to reduce the false positives rate. This will increase the potential for false negative findings which renders the screening ineffective.
Misconception #6. It is more sensitive to screen people one at a time.
Fact – The highest sensitivity and specificity is produced when a comparative analysis of all people being screened is used to establish a threshold and continually calibrate that threshold along with pattern recognition and any abnormal gradients.

Recent Comments